Vaccines have become the best-kept secret for saving lives in pediatrics. For better or worse, 21st-century Americans tend to underestimate vaccines because they have not personally experienced the devastation caused by vaccine-preventable diseases. The impact of vaccines on our society cannot be overstated. The ultimate public safety measure, vaccines have saved countless lives and improved the quality of life for humans in this country and around the world for more than two hundred years. Here is the heart of the problem. Because we are no longer surrounded by vaccine-preventable diseases, the importance of vaccines is easily underestimated by modern Americans.
A Historical Overview of Vaccine Preventable Diseases
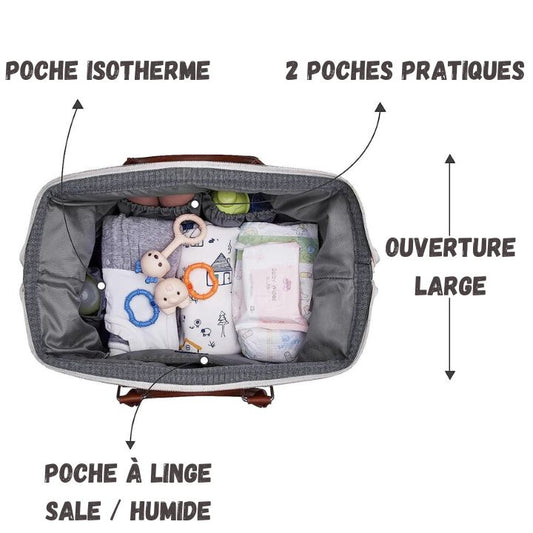
discover our Games & Toys collection.
A historical timeline of vaccine-preventable diseases helps illuminate the impact of vaccines on society. Before Edward Jenner developed the first smallpox vaccine in 1796, about 50,000 people in the United States developed smallpox each year, and about 1,500 died from it. Thanks to the vaccine, the disease was eradicated worldwide in 1977.
Before 1955, more than 16,000 people developed polio each year in the United States, and nearly 2,000 died from it. Of those who did not die, about 1 in 25 developed meningitis, and 1 in 200 suffered paralysis, sometimes permanently. Incidentally, my mother contracted polio and developed paralysis of her right arm as an infant in 1949, six years before Jonas Salk developed the first polio vaccine (Salk also developed the first flu vaccine in 1938). The last case of wild polio in the United States was diagnosed in 1979.
My grandmother, who immigrated to America in 1917, lost her little brother to measles during their transatlantic crossing. Before the vaccine became available in 1963, more than three million Americans suffered from measles each year, nearly 50,000 people were hospitalized, 4,000 developed encephalitis, and more than 400 died. Currently, in regions where vaccination rates are low, the disease is still very present. In 2014, there were approximately 267,000 cases of measles worldwide and 146,000 deaths, mostly among children. In 2016, mainly due to mass vaccination campaigns, the global rate of the disease fell to 90,000. This decrease represents an impressive decline of 84% over 16 years.
In the early 1990s, a large outbreak of measles occurred in cities across the United States (including LA, San Diego, Dallas, and NYC), resulting in nearly 30,000 total cases, the highest number in the recent history of our country. The disease spread rapidly among undervaccinated minority preschool children. More than 6,000 people suffered complications from measles, such as pneumonia, encephalitis and death.
A Personal Example
On a personal note, one of my oldest friends was affected by the NY outbreak. We both graduated from high school in 1990, and she was living in Poughkeepsie, NY at the time. Although the local DPH recommended revaccinating area children for better protection against measles, my friend was preparing to attend her prom and was concerned that the vaccine would leave an unsightly mark on her arm ( she was planning to wear a strapless dress and wanted to look her best). Sure enough, someone at the ball had measles, and she developed symptoms of the illness a few days later. Ironically, her parents, both doctors, did not think she might have measles, so they did not initially seek medical attention. A few days later, my friend was hospitalized in an intensive care unit with delirium and encephalitis. She almost died from a completely preventable illness.
The current situation
Nearly all cases of measles in the United States today are imported from other countries. Unfortunately, the disease continues to proliferate in regions where vaccination rates are low. In December 2014-January 2015, a measles outbreak infected 125 people in California, resulting in at least 17 known hospitalizations. The “Disney Land epidemic” was imported by an international visitor and perpetuated by low local vaccination rates. Forty-nine cases were not vaccinated, including 28 by parental choice, not because the children were too young to receive the vaccine. Similar outbreaks have occurred in other poorly vaccinated communities. In 2014, 383 people in an Amish community in Ohio developed measles after international exposure. Most patients (89%) were not vaccinated. These outbreaks show that measles remains a prevalent threat outside the United States and that undervaccination there leaves some American communities vulnerable to widespread infections. For this and other reasons, parents should remain vigilant about vaccinating children against measles and other preventable infectious diseases. Globally, the CDC estimates that for children born between 1994 and 2013, the measles vaccine will prevent 322 million illnesses, 21 million hospitalizations, and 732,000 deaths; Overall, the vaccine will save $295 billion in direct medical costs, plus another $1.38 trillion in societal costs.
Rubella and Other Diseases
Several years before the rubella vaccine was licensed in 1969, an epidemic affecting 12.5 million people occurred in America. Around 20,000 babies were born with congenital rubella syndrome: 11,000 were deaf, 3500 were blind and 1800 had intellectual deficits. This epidemic caused more than 11,000 miscarriages and resulted in more than 2,000 deaths. Since 2012, only 15 cases of rubella have been reported in this country.
In the early 1980s, hemophilic influenza was the leading cause of bacterial meningitis and postnatal brain damage in children, with approximately 20,000 total infections per year. In 1998, 13 years after the vaccine was approved, a total of 125 cases were reported in the United States. The bacteria once caused thousands of cases of life-threatening epiglottitis in children, but the disease has essentially been eliminated.
Chickenpox
Almost no one thinks of chicken pox, also known as chickenpox, as a devastating disease. But by the early 1990s, each year in America, the virus was infecting four million people, causing more than 10,000 hospitalizations and leading to 100 to 150 deaths. Over the past 15 years in my pediatric practice, I have encountered exactly ONE case of chickenpox. This child developed a severe secondary bacterial infection requiring antibiotics.
Streptococcus Pneumoniae
Before the pneumococcal conjugate vaccine was approved in 2000, Streptococcus pneumoniae caused 13,000 cases of bacteremia in children, 700 cases of meningitis, five million ear infections, and 200 deaths in America each year. Globally, pneumococcus was responsible for approximately 14.5 million serious infections per year and more than 800,000 deaths, particularly among children and the elderly. Although rates of the disease have fallen after the widespread use of several vaccines, it is important to recognize that pneumococcus remains a significant threat at home and abroad. Strep pneumo is currently responsible for approximately four million illnesses per year, nearly 500,000 hospitalizations and 22,000 deaths, especially among children and the elderly.
A Case of Personal Experience
Several years ago, in my office, I saw an almost two-month-old baby with a fever who was two days away from his first vaccination visit. This child had pneumococcal meningitis, a potentially fatal disease. Although he was treated quickly with antibiotics in hospital, he later developed deafness in both ears, a common complication of meningitis. Aside from the hepatitis B vaccine, which is administered in hospital, the first set of vaccinations is currently administered at two months of age, a time of life when the immune system is particularly vulnerable to serious infections like meningitis. New parents often ask my opinion on delaying vaccinations. My answer is always a resounding "No! Of course not!" Vaccines must be administered on time, NOT on alternate schedules. Young infants are at risk for significant infections with life-changing complications. Delaying vaccines in this age group (or any other age group, for that matter) opens the door to undesirable consequences. The baby who had meningitis, and his family, will face problems related to deafness for the rest of his life. Thinking about this case, I often wish that the pneumococcal vaccine would be licensed for administration immediately after birth. Indeed, one study demonstrated that "...doses [of pneumococcal vaccine] administered at birth were found to be immunogenic and primed for doses administered later."
Whooping cough
In the early 1920s, whooping cough, or “pertussis,” infected more than 200,000 people a year. Then and now, young infants are particularly vulnerable to disease and have the highest mortality rates. In 2016, seven children died from pertussis in the United States, and six of these patients were less than 1 year old. Like pneumococcus and influenza, pertussis is an example of an infection that is actively circulating throughout our country and internationally. In 2012, the most recent peak year in the United States, 50,000 cases of whooping cough were reported (the numbers are likely much higher, because many cases go undiagnosed and unreported). Immunity to the whooping cough vaccine unfortunately wanes over time, which helps explain why the disease is still so prevalent. Because infants cannot receive the pertussis vaccine until they are two months old, it is essential that pregnant women receive the Tdap vaccine, which protects against pertussis, tetanus and diphtheria. During pregnancy, maternal antibodies are passed to the baby through the placenta, and after delivery, the antibodies are transferred to the baby through breast milk, if the baby is breastfed.
Influenza
Because influenza ("influenza") is not a reportable illness, the data below is an estimate. From 2015 to 2016, influenza caused an estimated 9 to 35 million illnesses in the United States, 140,000 to 710,000 hospitalizations, and 12,000 to 56,000 deaths. Although vaccine effectiveness is unpredictable due to frequent mutations of the virus, the CDC estimates that the flu vaccine prevents five million illnesses per year, as well as 2.5 million health care-related visits, 71,000 hospitalizations and 3,000 deaths in this country.
A Lesson Learned
Years ago, when I was younger and more naive, I didn't particularly push families to get flu shots. Then a patient taught me a lesson. A previously healthy teenager, with no medical history, came into my office one winter evening with a cough and a fever of 105 degrees. A rapid flu test quickly confirmed he had the flu, but something was wrong. A spotted pink rash had appeared on his back, and his lung exam revealed some crackles. Reassuringly, his blood pressure and oxygen levels were completely normal. I asked the patient if he preferred to go home or go to the emergency room for a chest x-ray to rule out pneumonia. The patient's response was: "I want to go to the hospital." When a sick person says that, I never argue. So the patient and his mother left for the hospital. A few hours later, I received the terrible news that this patient was fighting for his life in intensive care. Shortly after arriving at the hospital, he had gone into septic shock due to a secondary bacterial infection (pneumonia caused by Staphylococcus aureus, a common complication of influenza) and required intravenous fluids and vasopressors to maintain his blood pressure. And I almost sent this patient home from my office! I am convinced that if he had gone home, he would have died that night in his bed. Thanks to divine providence, an intelligent mother and excellent medical care in intensive care, my patient ultimately survived the illness. These days, when someone asks me if healthy people really need a flu shot, I always say, “Yes!”
Incidentally, this case is no different than those we are hearing about in the media right now, during the 2017-2018 flu season. Although this year's flu vaccine is not a good match for circulating strains of the virus, studies show that people who contract the more virulent H3N2 variety will have a milder course if they have already received a vaccine against it. influenza.
The Cancer Vaccine of the 21st Century
One of the biggest killers of Americans in the 21st century is cancer. Given the heavy burden of cancer in this country and all the misery it causes patients and their families, you'd think most people would be quick to embrace a cancer vaccine. Nevertheless, it is not the case. The vaccine I am referring to is Gardasil. Although Gardasil was initially approved for the prevention of cervical cancer in 2006 (12 years ago in 2018), and the data supporting its use is now very strong, the vaccine is still refused by approximately 40% of families. Even before they come to my office, many parents have already decided that they do not want Gardasil, and nothing I say may change that opinion.
Like many other pediatricians, I find this frustrating, mainly because Gardasil turns out to be an incredibly important preventative public health measure for saving lives. Gardasil prevents human papillomavirus, or HPV. HPV is a sexually transmitted disease responsible for many cancers, including cancer of the cervix, vagina, vulva, penis, anus, rectum, and oropharynx. Wherever the virus can live, it can cause cancer. HPV has been called a “hidden epidemic,” which is an accurate description. According to the CDC, approximately 80-90% of American women and men will, at some point, be infected with HPV. Half of these individuals will acquire high-risk strains capable of causing recurrent disfiguring warts (either in the genitals or oropharynx) or cancer. Initially, HPV is a silent infection. Much like an initial HIV infection, most people don't realize they have contracted the virus. Importantly, sexual intercourse is NOT necessary for transmission. Physical skin-to-skin contact and oral sex can easily spread the virus, which has contributed to its ubiquity.
Gardasil: An Essential Vaccine
In total, HPV is directly responsible for nearly 32,000 cases of cancer each year in the United States, plus an even greater number of precancerous conditions requiring invasive treatment. Although there are many strains of HPV (about 40 are sexually transmitted, and 60 cause common warts), a small subset is responsible for causing genital warts and cancer. More specifically, nine aggressive strains (6, 11, 16, 18, 31, 33, 45, 52 and 58) are targeted by Gardasil. The vaccine is potentially capable of preventing more than 90% of cervical and anal cancers, as well as a high percentage of the other cancers mentioned above. It is important to recognize that the vaccine must be administered BEFORE exposure, before a person is sexually active. Once a person is infected with a cancer-causing strain of HPV, the vaccine can no longer protect against that strain.
In the United States, Gardasil is covered by insurance from ages 9 to 26. In my practice, I typically offer it to patients at age 12, mainly because children are not due for other vaccines at that time, and I like to make visits as pleasant as possible. . Because the immune response is so robust for young adolescents, they only need two shots to achieve 100% immunity. People over 16, however, need three vaccines.
Recent Data and Importance of Vaccination
On a positive note, recent data from Australia indicates that the HPV vaccine is already having a significant impact on disease rates. The rate of JORPP (juvenile recurrent respiratory papillomatosis), an incurable and potentially fatal respiratory disease in children caused by mother-to-child transmission of HPV at birth, is declining for the first time in history. The surveillance program in Australia detected a decline in incidence from 0.16 to 0.02 cases per 100,000 people from 2012 to 2016, the period corresponding to widespread HPV vaccination. This improvement is just the beginning of the positive change we will see as HPV vaccination becomes more common. Interestingly, in Australia, the vaccine is covered for people up to the age of 45. In my opinion, if an older adult is sexually active and not immune to HPV, then receiving the vaccine is a great idea. Out of pocket, one injection of Gardasil costs about $150, and three injections are needed to vaccinate people who start the series later. Although it is not cheap, the cost of receiving three Gardasil vaccines is much lower than the cost of treating cancer.
Which brings us back to the puzzling question: Why do so many parents routinely reject Gardasil in pediatric offices across the country?
Since vaccines were first developed, people have spoken out against them due to a combination of distrust, misunderstanding, and disbelief. The Anti-Vaccination League and the Anti-Compulsory Vaccination League, for example, emerged in the mid-1800s in response to laws making smallpox vaccination compulsory. In general, new concepts and technologies are frequently rejected at their creation (climate change, anyone?). The practice of questioning scientific proclamations is robust in America, and that's not necessarily a bad thing. On the other hand, our public education system seeks to develop critical thinking skills. Instead of blindly accepting authority, we are taught to examine the evidence and form our own opinions. But at some point, solid scientific data must lead to definitive conclusions. Yet people rationalize or reject this data when it conflicts with the core tenets of their worldview. Additionally, critical thinking can break down when inaccurate information enters the fray, muddying the waters, making it difficult or impossible to reach informed conclusions.
Lies about Vaccines
One of the murkiest times for vaccines came in 1998, when Dr. Andrew Wakefield published an article in The Lancet claiming that the MMR vaccine caused autism in children. Although Wakefield's data was found to be fraudulent and he was completely discredited, the article caused lasting damage to the general public's faith in vaccinations. If you are someone who has doubts about vaccines and autism, I am happy to report that a multitude of scientific studies are completely reassuring. In 2012, the Cochrane Library published a review article including approximately 14,700,000 children that showed absolutely no link between vaccines and autism. Other large studies have reached the same conclusion, again and again.
If you're still not convinced, you're probably spending too much time on the Internet. On the web, anyone can say anything. Here are some common untruths you might find there.
Untruths about Gardasil:
- Gardasil is part of a government conspiracy to sterilize our population.
- Gardasil causes paralysis.
- It is not safe to receive Gardasil.
- The Gardasil vaccine has killed people. Fake. No one has ever died from a Gardasil vaccine (see below).
- Giving Gardasil to your child will encourage them to have sex at a young age.
Untruths about vaccines in general:
- Vaccines weaken the immune system. Fake. They strengthen the immune system by increasing our reserve of antibodies.
- The injectable flu vaccine causes the flu. Fake. The current flu vaccine is 100% inactivated. Yes, you might feel tired for a day or two after the shot, and your arm might be a little sore, but you CANNOT get the flu from an injectable flu shot.
- Vaccines cause autism. False, see above.
- Vaccines are a conspiracy perpetrated by Big Pharma. Wrong again! Although pharmaceutical companies make money on vaccines, they represent a tiny portion of overall profits; furthermore, immunization prevents diseases that would require treatment with other, much more expensive drugs if the diseases were allowed to run their course. Gardasil, for example, prevents a multitude of cancers that would require expensive treatments and chemotherapy drugs. In general, preventing disease makes Big Pharma less money than letting disease devastate.
- Alternative vaccination schedules are good for children because receiving three or four vaccines at the same time can overwhelm the immune system. A concise article written by Dr. Mark Crislip and Dr. Stephen Barnett strongly refutes this erroneous conclusion. They explain that a human immune system is capable of producing around 10 billion antibodies. Over the course of a lifetime, most people will produce approximately 1 to 100 million antibodies. Collectively, childhood vaccines induce the production of only 30 antibodies. Theoretically, we should receive 10,000 vaccines at a time to reach our immunological capacity. On a related point, I would never recommend delaying vaccines or using alternative schedules for young infants. Younger infants, especially those younger than three months, are particularly vulnerable to life-threatening infections, such as meningitis.
- You can trust the anti-vaccine information on Dr. Joseph Mercola's website. FALSE, with a capital F. Websites like Mercola's are dangerous because the information presented appears scientific and well-reasoned, but is not based on scientific fact. “Pseudoscience” websites like this twist data with the intention of manipulating public opinion. The Mercola website, for example, claims that Gardasil has caused more than 200 deaths. Despite the information listed here and on many other websites, Gardasil has not caused any deaths. Think of it this way: for living people, the risk of death is 100%. Because some people die at a young age, a certain percentage of HPV vaccinated individuals will die shortly after receiving the vaccine (eventually, 100% of them will die). But that doesn't mean Gardasil caused their deaths. Mercola's website is filled with equally misleading information. If no one believed it, no problem; but some parents who visit websites like Mercola's will refuse Gardasil, needlessly putting their children at risk of cancer.
- The mercury preservative used in vaccines is dangerous. No, this is not the case. Additionally, other than the multidose flu vaccine, childhood vaccines no longer contain mercury. The last childhood vaccines containing mercury were withdrawn in 2003.
- Aluminum adjuvant in vaccines is dangerous. It causes Alzheimer's disease and breast cancer. Still wrong, on every point! Aluminum is a ubiquitous element that people ingest daily through food and drinking water. Most of the aluminum we consume passes through the digestive tract without being absorbed. Every day, people swallow around 10 to 100 mg of aluminum. Over a one-year period, the most aluminum a baby could receive through vaccines is about 4.2 mg, a tiny and safe dose.
- Getting measles is no big deal. If my child gets measles, she will receive excellent medical care in an American hospital. Nothing bad could happen. Fake ! Even with excellent medical care, people infected with measles still have many complications.
- 1 in 20 develop pneumonia, the most common cause of death
- 1 in 10 develop ear infections, which can cause permanent hearing loss
- 1 in 4 require hospitalization
- 1 in 1,000 develop encephalitis (like my friend from Poughkeepsie, NY, who once refused a measles vaccine during a local outbreak); encephalitis can cause deafness and permanent neurological disabilities
- 1 to 2 in 1000 will die
Conclusion
My parents didn't vaccinate me, and I've never been sick, so why should I vaccinate my children? You've never been sick because everyone around you is vaccinated. In other words, you are protected by “herd immunity”. Plus, you are an N of 1. Just because you haven't gotten sick doesn't mean your kids won't.
Vaccines are an essential tool for public health, and it is crucial that we continue to vaccinate our children to protect not only themselves but also our community as a whole. For more information on the importance of vaccines and official recommendations, you can consult the Vaccination Info Service website of the Ministry of Solidarity and Health.